Histamine and Sleep Connection – A Low-Histamine Evening Protocol for Unexplained Night Wakings
Concise Summary:
Many people suffer from unexplained night wakings despite practicing good sleep hygiene. A lesser-known trigger may be histamine—a compound that plays a role in both immune response and brain arousal. As a neurotransmitter, histamine can heighten alertness and disrupt sleep when elevated at night. This article explains the link between histamine and sleep and offers a practical low-histamine evening protocol including dietary tips, environmental adjustments, and natural supplements. By lowering histamine exposure in the evening, people with insomnia or night wakings may finally experience deeper and more restorative sleep.
Introduction
Sleep is essential for physical and mental health, influencing everything from cognitive function and mood stability to hormonal balance, digestion, and immune resilience. Despite following recommended sleep hygiene — such as maintaining a consistent bedtime, limiting screen exposure, or optimizing the bedroom environment — many still wake up during the night without explanation. These midnight awakenings can be disruptive and frustrating.
One overlooked factor that may be responsible for these disturbances is histamine, a molecule typically associated with allergic symptoms like sneezing or skin irritation. However, histamine also plays a critical role in the brain as a neurotransmitter that maintains alertness.
When histamine is elevated at night, it may overstimulate the body’s nervous system just when it should be winding down, leading to sleep fragmentation. This article explores the relationship between histamine and sleep, and introduces a low-histamine evening routine designed to calm the system and promote longer, more restful sleep.
The Science: Histamine’s Role in Sleep Regulation
Histamine serves two primary roles in the body:
1. As a key player in immune response, helping the body fend off allergens.
2. As a neurotransmitter, promoting wakefulness and alertness.
In the brain, histamine originates in neurons located in the tuberomammillary nucleus of the hypothalamus. These neurons project to numerous brain areas involved in attention, arousal, and mood regulation. When histamine remains elevated in the evening or overnight, it can keep the brain in a hyper-alert state, preventing entry into deeper non-REM and REM stages of sleep.
A study from The Journal of Pharmacology and Experimental Therapeutics (2002) found that blocking H1 histamine receptors in animals led to deeper non-REM sleep. This explains why common antihistamines — especially first-generation ones like diphenhydramine — cause drowsiness: they suppress histamine’s arousing effects in the brain.
People with histamine intolerance often lack sufficient levels of DAO (diamine oxidase), the enzyme responsible for breaking down histamine from food. Symptoms can include digestive issues, skin sensitivity, and notably — sleep disruptions. According to a study published in Nutrients (2018), a low-histamine diet reduced insomnia and improved sleep quality in patients with histamine intolerance.
Children with high histamine conditions like eczema, allergic rhinitis, or ADHD-like attention difficulties often wake up multiple times each night. This highlights how both adults and children may benefit from interventions aimed at moderating histamine levels before bed.
Even without overt allergic symptoms, elevated nighttime histamine may hinder restorative sleep, influencing brain wave activity and reducing the proportion of deep and REM sleep. Therefore, effectively managing histamine levels before and during sleep may be an essential — yet underrecognized — element of good sleep hygiene.
A Low-Histamine Evening Protocol for Better Sleep
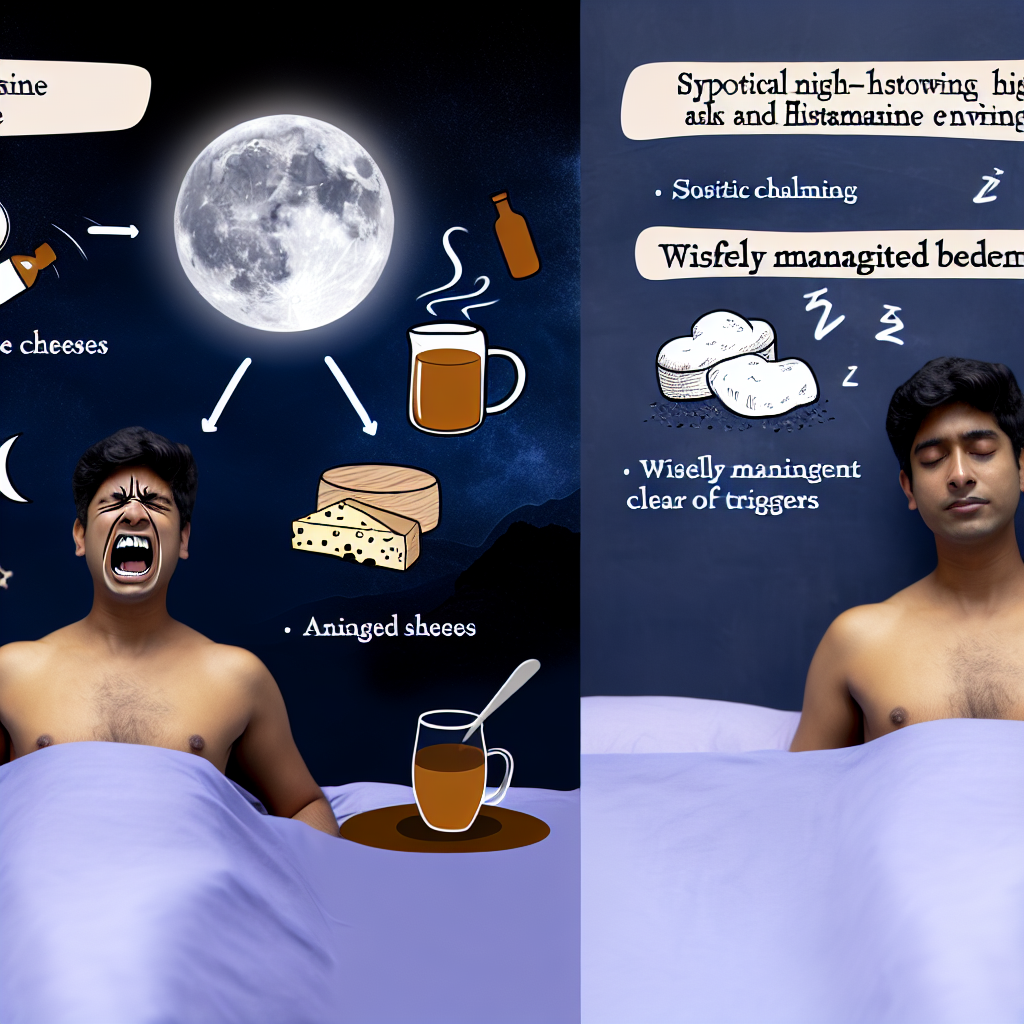
Adopting a low-histamine bedtime routine involves both dietary changes and environmental modifications. Here’s a comprehensive, practical guide for adults and children.
1. Avoid High-Histamine Foods in the Evening
Many common foods are either naturally high in histamine or stimulate the body to release more of it. Avoid these in your dinner or post-dinner snack:
– Aged cheeses (e.g., parmesan, cheddar, blue cheese)
– Fermented foods (e.g., kimchi, yogurt, pickles, miso)
– Processed or smoked meats (e.g., ham, sausage, pepperoni)
– Leftovers, especially meats left in the fridge more than a day
– Condiments with vinegar (e.g., ketchup, mayonnaise)
– Alcohol — especially wine, beer, and champagne
– Chocolate and tomatoes (moderate histamine content and liberators)
Safer evening food alternatives include:
– Freshly prepared meats or eggs (avoid slow-cooking or rewarming)
– Cooked white rice, quinoa, or sweet potatoes
– Steamed leafy veggies (spinach, romaine, collards)
– Fresh fruits like blueberries, apples, and pears
– Herbal teas such as chamomile, rooibos, lemon balm
Eating high-histamine meals too late in the day can elevate blood histamine levels just as the body is preparing for rest. Evening food choices set the tone for sleep quality.
2. Manage Your Environment
Even if your indoor spaces feel “clean,” unseen exposures to environmental allergens can silently raise histamine. Dust mites, mold spores, pet dander, and pollen may not trigger sneezing during the day, but can result in histamine surges at night and lead to sudden wake-up periods.
Effective practices include:
– Use air purifiers with HEPA filters
– Wash bedding and pillowcases weekly in hot (130°F) water
– Use encasements certified to block dust mites on pillows and mattresses
– Remove stuffed animals or plush decor from children’s sleeping areas
– Keep pets and indoor plants out of the bedroom
– Maintain 40–50% humidity (use a dehumidifier if needed)
3. Wind Down Naturally
The transition from high daytime stimulation to sleep needs to be deliberate. Excess cortisol and neurological stimulation in the evening can aggravate histamine pathways.
Suggestions for winding down include:
– Avoid screens for at least 60–90 minutes before sleep
– Try low-light reading, sketching, or gratitude journaling
– Practice breathwork, progressive muscle relaxation, or guided sleep meditations
– Take a warm bath with Epsom salts 30–60 minutes before bed to relax the nervous system
Many of these actions also support production of melatonin and reduction in central nervous system stimulation.
4. Support DAO Enzyme Function
Boosting the enzyme DAO — your body’s natural defense against histamine — can improve tolerance and reduce circulating histamine levels.
Helpful nutrients for DAO support include:
– Vitamin C: Found in bell peppers, kiwi, or taken as a supplement
– Vitamin B6: Found in bananas, chicken, or oats
– DAO supplements: Can be taken 15–30 minutes before histamine-containing meals (consult a healthcare provider for the correct dosage)
Dehydration can reduce DAO function, so ensure adequate water intake throughout the day but reduce fluids an hour before bed to avoid waking up to urinate.
5. Antihistamines – With Caution
Occasional use of sedating antihistamines like diphenhydramine (Benadryl) or hydroxyzine may help break the cycle of night wakings for some, especially when histamine overload is clearly suspected.
However, frequent reliance can create dependency, alter sleep architecture, and worsen grogginess in the morning. Discuss any regular use with a healthcare provider, especially for children or those with known histamine sensitivity.
Conclusion
While sleep disturbances can have many sources, the role of histamine in sleep regulation is a scientifically validated — yet under-acknowledged — contributor to insomnia and frequent night wakings. Elevated nighttime histamine can cause sleep fragmentation, light sleep stages, and a lack of restorative rest, even without obvious daytime allergy symptoms.
By making intentional shifts in food choices, environmental factors, and lifestyle rhythms, we can significantly lower evening histamine exposure. Whether it’s for a child waking every two hours or an adult struggling with unexplained insomnia, a low-histamine evening protocol offers a gentle, science-informed path to deeper and more continuous sleep.
Track your progress with a sleep and diet journal and work with a healthcare provider if symptoms persist or worsen. With consistency and curiosity, restful sleep may be just a few changes away.
References
– The Journal of Pharmacology and Experimental Therapeutics (2002). “Histamine H1 Receptor Antagonist Effects on Sleep Architecture.”
– Nutrients (2018). “Histamine Intolerance and Its Spectrum of Symptoms: Causes, Diagnosis, and Treatment.”
– National Institute of Neurological Disorders and Stroke. “Brain Basics: Understanding Sleep.”
– National Library of Medicine. “Histamine and Sleep-Wake Regulation.”
For more tips on science-backed sleep strategies, visit our resources on MedOze.com.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com