Sleep Apnea Pre-Habilitation – Breathing and Myofunctional Exercises to Support PAP Therapy
Sleep apnea, a prevalent and often undiagnosed sleep disorder, undermines not only restorative sleep but also overall well-being, **cognitive function**, and cardiovascular health. The most common form—Obstructive Sleep Apnea (OSA)—occurs when soft tissues of the upper airway collapse intermittently during sleep, disrupting breathing and lowering oxygen levels. The standard treatment for OSA is Positive Airway Pressure (PAP) therapy, wherein a machine delivers continuous airflow through a mask, ensuring the airway remains open.
While PAP therapy is clinically proven to reduce OSA symptoms, many patients struggle with discomfort, mask fit issues, pressure intolerance, or simply the psychological barrier of using a device every night. These challenges often lead to inconsistent use or complete abandonment of therapy. Recognizing this, sleep medicine has begun to adopt pre-habilitation—a proactive approach emphasizing physical and functional preparation prior to starting therapy.
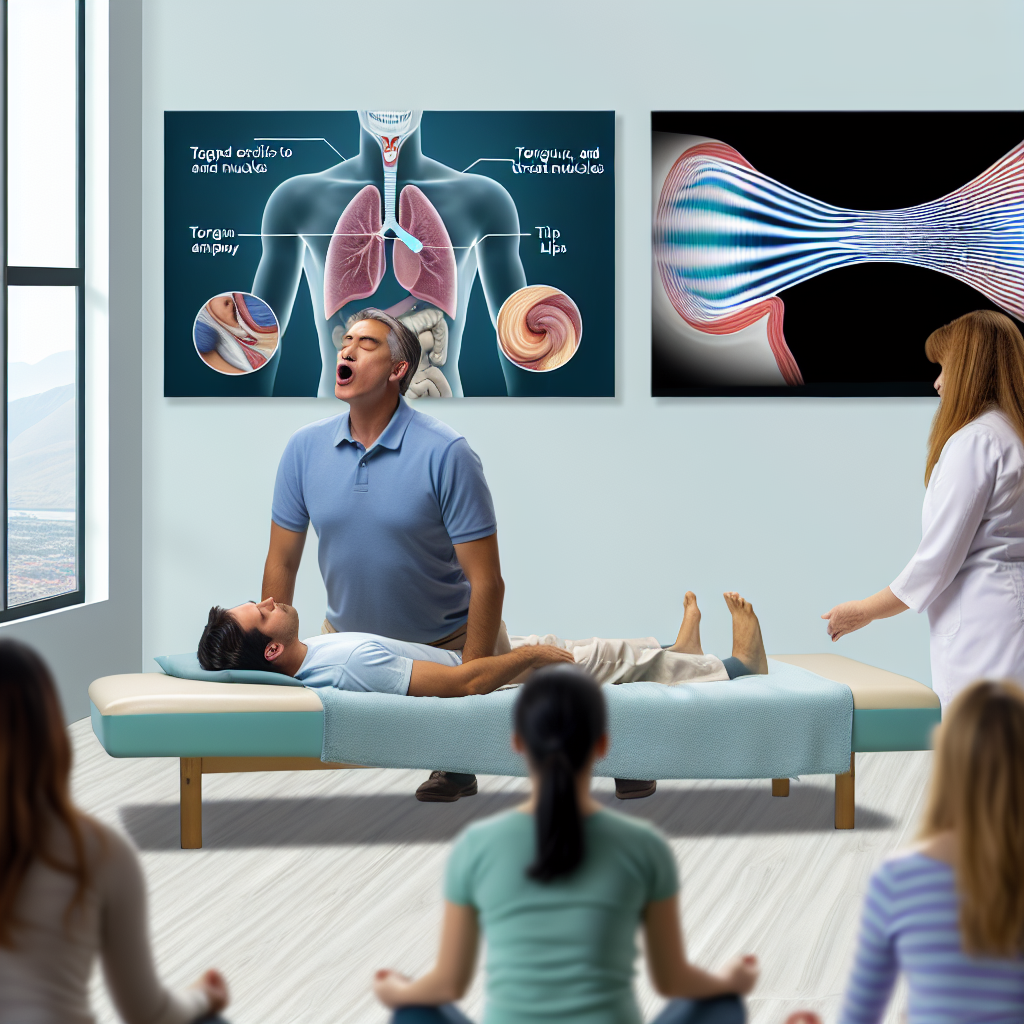
Sleep apnea pre-habilitation integrates breathing retraining and orofacial myofunctional therapy (OMT). These structured programs condition the oral and pharyngeal muscles while instilling healthier breathing patterns, enhancing airway tone, and promoting nasal breathing. Patients who engage in pre-habilitation often experience easier adaptation to PAP, better comfort, improved mask seal, and even reduced pressure settings.
Strengthening key muscle groups—like the tongue, soft palate, lips, and throat—reestablishes functional stability in the airway during sleep. On the other hand, habitual mouth breathing, weak airways, or poor respiratory coordination can exacerbate OSA symptoms. Thus, correcting dysfunctional behaviors with targeted exercises not only improves sleep quality but also optimizes PAP therapy results.
Importantly, this integrative strategy is safe and beneficial for individuals across all ages—from children showing early signs of disrupted sleep to adults recently diagnosed with OSA. By engaging patients actively in their treatment journey, pre-habilitation bridges the divide between “passive device use” and “active airway health improvement.”
Features and Supporting Research
Clinical research confirms that the success of PAP therapy is not dependent solely on machine specifications—it is greatly influenced by the patient’s upper airway muscle tone and current breathing mechanics. Reduced functionality in these areas often correlates with lower adherence and treatment failure.
A foundational study by Guimarães et al. (2009) published in the journal Sleep demonstrated that daily oropharyngeal exercises can significantly reduce OSA severity. In this three-month trial involving participants with mild to moderate OSA, exercises used to strengthen the tongue, soft palate, and face led to a 39% reduction in Apnea-Hypopnea Index (AHI), a key measure of OSA severity. Additionally, participants reported lower snoring intensity and sleepiness, signaling an improvement in both physiological and symptomatic outcomes.
A comprehensive meta-analysis by Camacho et al. (2015) in Sleep Medicine Reviews further underscored the benefits of myofunctional therapy. Across nine studies and over 250 patients, consistent improvements were documented in AHI, oxygen levels, and sleep quality. Importantly, those who combined these exercises with PAP therapy showed enhanced adherence and greater long-term treatment success due to improved tolerance and reduced pressure requirements.
Equally vital is nasal breathing retraining. Techniques like the Buteyko method encourage slow, nasal-dominant breathing, improving CO2 tolerance and respiratory balance. In a publication by Courtney R. (2011) in Breathe, nasal retraining proved effective in increasing oxygenation and minimizing symptoms associated with disordered breathing. Transitioning from mouth to nasal breathing not only optimizes oxygen delivery but also supports airway stability throughout the night.
Notably, children with obstructive sleep symptoms also benefit from early myofunctional intervention. Research by Guilleminault et al. (2004) in The Laryngoscope found that post-surgical children who practiced myofunctional therapy post-adenotonsillectomy had fewer recurrences of OSA and better long-term airway development. This highlights the potential for early, conservative interventions to reduce dependence on devices like PAP or even repeat surgeries.
Beyond physiological improvements, incorporating these exercises also impacts psychological well-being. Patients often feel more in control, empowered, and optimistic about their recovery. Myofunctional and breathing exercises promote self-efficacy, reduce performance anxiety related to PAP, and foster affirmative behavioral changes necessary for lifelong sleep hygiene.
Conclusion
Obstructive Sleep Apnea (OSA) presents a multilayered challenge. While PAP therapy remains the gold standard, its efficacy is tightly linked to patient compliance, which in turn hinges on comfort, respiratory strength, and behavioral adaptation.
Pre-habilitation—through structured breathing exercises and muscle training—is a validated, non-invasive solution to improve airway function and aid PAP acceptance. By restoring optimal muscle tone and advancing nasal breathing habits, these exercises empower patients to actively participate in their healing process.
Whether used in adults initiating PAP therapy, or children progressing through post-surgical recovery, sleep apnea pre-habilitation bridges passive treatment with active restoration. It offers a sustainable path forward in a multi-pronged approach to sleep health. As interest in holistic care grows, integrating myofunctional and breathing techniques into routine management will become increasingly standard—and appreciated—by both clinicians and patients.
Concise Summary
Sleep apnea pre-habilitation uses breathing retraining and myofunctional therapy to strengthen airway muscles, enhance nasal breathing, and improve adherence to PAP therapy. Evidence from clinical studies shows that these exercises reduce OSA severity, improve comfort, and foster patient engagement—especially important for children and new PAP users. This integrative, non-invasive approach proactively prepares patients for successful long-term management of sleep apnea.
References
-
Guimarães, K. C. et al. (2009). Effects of oropharyngeal exercises on OSA. Sleep, 32(5), 581–587.
-
Camacho, M. et al. (2015). Myofunctional therapy meta-analysis. Sleep Medicine Reviews, 25, 123–139.
-
Courtney, R. (2011). Buteyko method and breathing retraining. Breathe, 7(1), 47–54.
-
Guilleminault, C. et al. (2004). Myofunctional therapy in children. The Laryngoscope, 114(8), 1320–1324.
For more expert-backed resources on sleep apnea, pap therapy, and myofunctional breathing solutions, visit https://medoze.com.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com