Advanced PAP Therapy Integration – Solutions for Mask Discomfort, Air Leaks, and Dry Mouth
Introduction
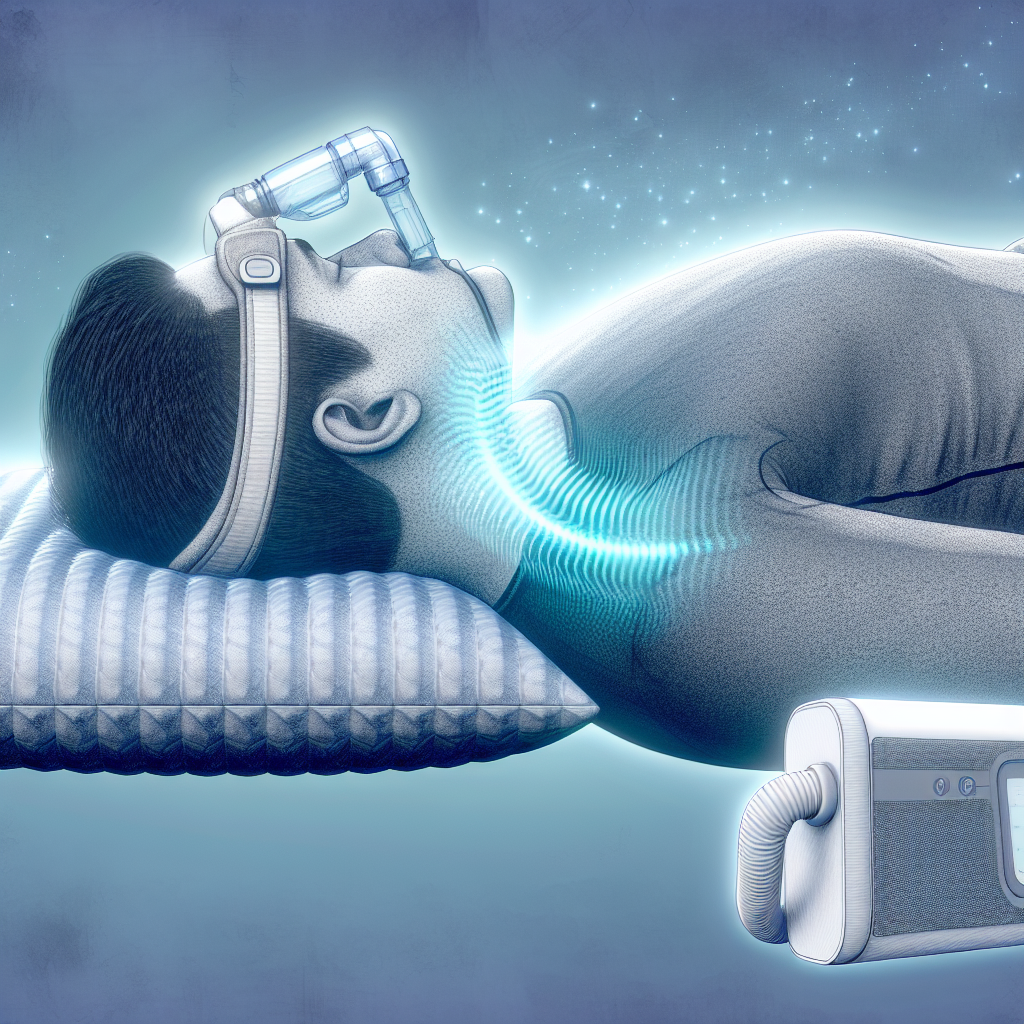
Positive Airway Pressure (PAP) therapy remains the gold standard for treating obstructive sleep apnea (OSA), a condition impacting roughly 22 million Americans. Unfortunately, nearly 80% of moderate to severe cases remain undiagnosed. Even among diagnosed individuals, adherence to prescribed therapies—including CPAP, BiPAP, and APAP—remains problematic due to physical side effects and discomfort.
Common concerns such as mask discomfort, air leaks, and dry mouth not only diminish quality of sleep but can also lead to therapy discontinuation. This is troubling, as untreated sleep apnea significantly increases risks of cardiovascular disease, metabolic disorders, and cognitive decline.
Fortunately, a wave of technological advancements and integrated care strategies is reshaping PAP therapy. These cover everything from adaptive humidification to smart mask fitting protocols and remote monitoring tools, enabling clinicians to personalize treatment. The result is improved comfort, greater compliance, and better long-term outcomes for patients.
Features of Advanced PAP Therapy Integration
1. Mask Discomfort Solutions
The effectiveness of PAP therapy greatly depends on a comfortable and properly fitted mask. According to the American Academy of Sleep Medicine (AASM), comfort directly affects adherence. Research published in the Journal of Clinical Sleep Medicine shows that soft cushion materials—such as gel or memory foam—along with ongoing adjustments based on user feedback, lead to higher tolerance and continued use.
Advanced designs from brands like ResMed (AirFit F30i) and Philips (DreamWear) accommodate diverse facial structures better by offering full-face, nasal, and nasal pillow masks. They reduce points of contact and minimize skin irritation—features crucial for those who sleep on their sides or have facial sensitivities.
2. Air Leak Management
Air leaks remain a primary cause of therapy inefficacy and reduced comfort. A 2020 study in Nature and Science of Sleep emphasized the importance of a secure but flexible mask fit.
Innovations like auto-leak detection in APAP machines automatically alert users or adjust pressure levels to compensate. Devices now offer gender-specific and pediatric masks, ensuring a customizable experience. Additionally, new mask materials—such as hybrid silicone-fabric combinations—allow masks to conform to facial movements during sleep without compromising the seal.
3. Dry Mouth and Humidification
Roughly 40% of PAP users report experiencing dry mouth, particularly those using nasal masks or those who habitually breathe through their mouths. Research in the Sleep and Breathing Journal highlights this as a significant barrier to long-term use.
Today’s machines combat dry mouth with integrated heated humidifiers and heated tubing systems. Devices such as ResMed’s ClimateLineAir and Fisher & Paykel’s ThermoSmart system offer adaptive humidification, which adjusts moisture levels in real-time based on room climate and patient feedback. This avoids both over-humidification and under-humidification, promoting uninterrupted sleep and reducing oral discomfort.
4. Remote Monitoring and Data Integration
Smart PAP systems such as ResMed’s AirView or Philips’ EncorePlatform enable clinicians to monitor therapy remotely. These platforms provide real-time data on AHI (Apnea-Hypopnea Index), leak rates, pressure levels, and mask usage patterns.
According to a 2022 study in Sleep Medicine Reviews, remote monitoring enhances user satisfaction and boosts adherence, especially during the initial months of therapy. Integration with health apps and wearable tech allows users to stay informed and gives healthcare providers insight into daily usage trends, enabling preemptive troubleshooting.
5. User Education and Cognitive-Behavioral Therapy (CBT)
While equipment upgrades address physical concerns, behavioral challenges are also a major factor in therapy success. Cognitive-Behavioral Therapy for PAP adherence (CBT-PAP), as supported by evidence in the Chest Journal, helps patients overcome fears, misconceptions, and perceived burdens of therapy.
Educational programs delivered via telehealth or in-person sessions have been shown to significantly increase compliance. Topics covered include acclimating to masks, understanding therapy benefits, how to track progress, and troubleshooting discomfort. When patients understand both the “how” and “why” of PAP therapy, they are far more likely to stay committed long-term.
Conclusion
Thanks to advanced PAP integration, users now experience fewer therapy interruptions and discomforts. Solutions targeting mask discomfort, air leaks, and dry mouth have markedly improved—with help from responsive machines, better mask materials, and interactive patient care models.
Patients are now empowered through adaptive technology, remote data access, and behavioral interventions. As therapy becomes more personalized, sustained PAP compliance is within reach for a greater population. Individuals experiencing difficulties should consult specialists, update their equipment, and make use of educational and digital tools to maximize treatment success.
Concise Summary
Advanced PAP therapy now offers personalized solutions to mask discomfort, air leaks, and dry mouth—common issues that hinder treatment for obstructive sleep apnea. Utilizing adaptive humidification, smarter mask designs, and remote monitoring, patients experience improved comfort and greater adherence. Innovations like cushion-based masks, automated leak adjustments, and CBT-driven support ensure PAP success is more attainable, especially with modern telehealth and wearable integrations. Those struggling with therapy can benefit by exploring newer devices and engaging in ongoing education, ensuring long-term health and restful sleep.
References
– American Academy of Sleep Medicine. (2021). Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea.
– Jordan, A. S., McSharry, D. G., & Malhotra, A. (2014). Adult obstructive sleep apnoea. The Lancet, 383(9918), 736-747.
– Rotenberg, B. W., Murariu, D., & Pang, K. P. (2016). Trends in CPAP adherence over twenty years of data collection. Journal of Otolaryngology – Head & Neck Surgery, 45(1), 43.
– Bakker, J. P., & Weaver, T. E. (2019). Adherence to CPAP: what should we be aiming for? Chest, 155(6), 1272–1287.
– Smith, I., Lasserson, T. J., & Wright, J. J. (2020). CBT for sleep apnea adherence. Sleep Medicine Reviews, 50, 101247.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com