Post-Concussion Sleep Recovery Protocol – Supporting Neural Repair Through Regulated Rest
Introduction – Understanding Sleep’s Critical Role in Concussion Recovery
A concussion is not just a simple head injury—it is a form of mild traumatic brain injury (mTBI) that initiates complex neurological disruptions. These disruptions affect not only cognition, motor skills, and mood, but also deeply impact sleep cycles. While the recommendation to “get plenty of rest” is common following a concussion, current research shows that regulated, quality sleep is a vital component in healing the brain.
Sleep supports multiple healing mechanisms, such as neuroregeneration, clearing of metabolic waste, inflammation reduction, and neurochemical re-balancing. The most critical restorative activities occur during deep NREM and REM sleep.
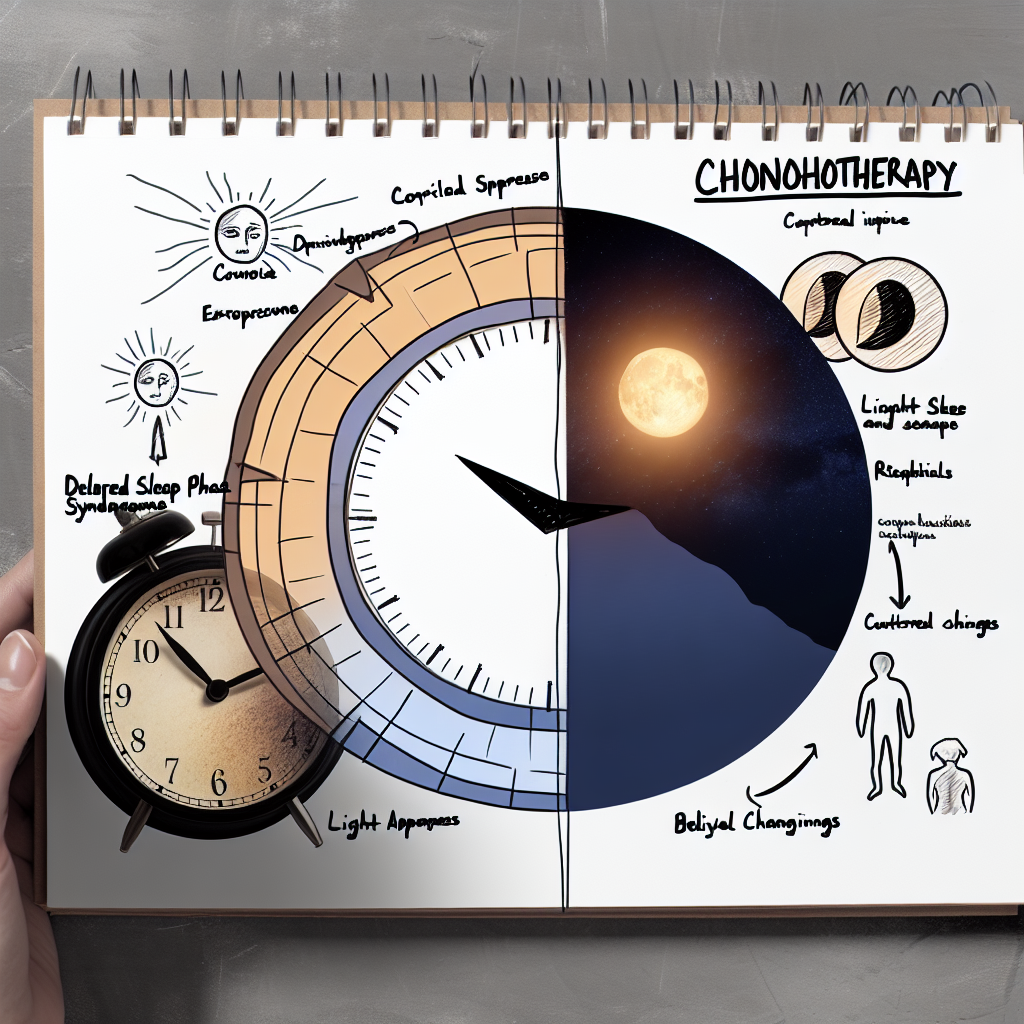
However, after a concussion, sleep itself often becomes impaired. Individuals may suffer from insomnia, excessive sleepiness, fragmented sleep, or a disrupted circadian rhythm. These disruptions can significantly delay recovery or lead to chronic post-concussion syndrome.
Additionally, this relationship is reciprocal. Poor sleep doesn’t just result from a concussion—it can worsen the condition by slowing neural repair and increasing cognitive fatigue. Because of this, clinicians are now emphasizing an integrated sleep recovery protocol as part of post-concussive care to optimize healing and prevent long-term complications.
Features – Scientific Insights Behind Sleep and Concussion Recovery
Recent studies have emphasized how sleep quality directly impacts recovery outcomes. A 2018 study in the Journal of Neurotrauma showed that patients with consistent, restorative sleep recovered significantly faster after a mild traumatic brain injury. In a 2019 review from Frontiers in Neurology, sleep disruptions were found to be among the strongest predictors of sustained concussion symptoms in children.
A key component of sleep’s healing power lies in the glymphatic system—the brain’s detox system. A seminal study in Science (2013) revealed that this system becomes active during deep NREM sleep, flushing toxins such as beta-amyloid and tau proteins—both associated with inflammation and neurodegeneration.
Injuries that disrupt circadian rhythms also lower melatonin levels. Melatonin is crucial not only for initiating sleep but also for its neuroprotective effects. Findings from Experimental Brain Research (2021) show that melatonin supplementation improved sleep cycles and cognitive outcomes in animal models following brain injury, suggesting similar potential in human treatments.
Adolescents are particularly susceptible. Research in Pediatrics (2016) found that high school athletes who slept fewer than eight hours post-concussion were over twice as likely to report prolonged symptoms.
There is broad agreement within the clinical community on the importance of personalized sleep interventions. These include sleep hygiene education, cognitive behavioral therapy for insomnia (CBT-I), strategic use of light, and even wearable tech to track recovery progress.
Objective assessments like actigraphy and polysomnography can detect subtle disruptions that subjective reports may miss—such as reduced slow-wave sleep or altered REM architecture—even when sleep duration appears normal.
Post-Concussion Sleep Recovery Protocol: Evidence-Based Practices
The following sleep-centric strategies can aid in brain recovery after concussion:
1. Immediate Rest and Gradual Reintegration
Begin with full physical and cognitive rest for 24–48 hours post-injury. After that, introduce light activities (e.g., reading, walking) as tolerated, ensuring they do not worsen symptoms.
2. Consistent Sleep-Wake Schedule
Go to bed and wake up at the same time every day. Consistency regulates your biological clock, reinforcing melatonin secretion and stabilizing energy rhythms.
3. Controlled Light Exposure
Natural light in the morning primes your brain for alertness, while limiting blue light before bed helps cue the body for melatonin release and rest.
4. Sleep Hygiene Optimization
Sleep in a quiet, cool, dark room. Avoid caffeine after 2 p.m., and stop eating heavy meals three hours before bed. Wind down with relaxing activities like stretching or soft music.
5. Melatonin Supplementation (with Medical Guidance)
In adolescents especially, carefully administered melatonin can help reset sleep cycles. Always consult a healthcare professional to determine proper dosage and duration.
6. Cognitive Behavioral Therapy for Insomnia (CBT-I)
A first-line treatment for post-injury sleep issues, CBT-I can replace negative sleep thoughts and behaviors with productive routines—without medication reliance.
7. Monitor and Adjust with Technology
Use devices like Oura Rings, Fitbit, or Apple Watch to track sleep duration, efficiency, and patterns. Share this data with professionals to guide your recovery plan.
8. Avoid Daytime Napping (If Possible)
While rest is important, extended or irregular naps can disrupt nighttime sleep. Limit naps to 20–30 minutes in the early afternoon if needed.
9. Collaborate with Specialists
Consult a sleep medicine specialist or neurologist if sleep changes persist beyond three weeks post-injury. Sleep studies may be needed to uncover hidden disturbances.
Conclusion – Rest as a Neurological Prescription
Although concussions don’t often leave visible signs, they can deeply disrupt the brain’s inner workings—especially regarding sleep regulation. The emerging science is clear: quality sleep is not just helpful but essential in concussion recovery.
Post-concussion care must move beyond generalized “rest” and embrace a structured, validated sleep recovery protocol. With proper environmental changes, medical interventions, and behavioral therapies, we can harness the brain’s natural repair system most effectively—through regulated rest.
Whether you’re a caregiver, patient, or healthcare provider, remember: successful healing from a concussion always begins—and ends—with good sleep.
Concise Summary
A concussion disrupts brain function, often impairing sleep—a vital element for neural repair. Quality sleep facilitates inflammation control, detoxification, and cognitive recovery. However, disturbances like insomnia and circadian disruption can persist after brain injury, complicating healing. A structured sleep recovery protocol—including consistent schedules, light management, CBT-I therapy, and possible melatonin use—should be part of every post-concussion treatment plan. Recent studies confirm the essential role of regulated sleep in promoting faster recovery and reducing long-term effects. Addressing sleep disturbances directly is key to full neurological rehabilitation and long-term well-being after a concussion.
References
– Journal of Neurotrauma (2018) – Sleep Quality and Recovery After Mild Traumatic Brain Injury
– Frontiers in Neurology (2019) – Predictors of Persistent Post-Concussion Symptoms
– Science (2013) – Sleep Drives Metabolite Clearance from the Brain
– Experimental Brain Research (2021) – Melatonin and Sleep Disturbances Following Traumatic Brain Injury
– Pediatrics (2016) – Insufficient Sleep Increases Post-Concussion Symptoms in Adolescents

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com